Tennessee has one of the nation’s highest cancer mortality rates. A partnership between the University of Tennessee, Knoxville, the UT Health Science Center, and Oak Ridge National Laboratory aims to improve outcomes for cancer patients by identifying new precision therapies that leverage the state’s deep expertise in radioisotope production.
The partnership will advance new radioisotope theranostics—diagnostics plus therapeutics—from concept to clinical application by combining the talents and resources of each organization’s scientists and clinicians.
“We’re building on our existing expertise to position our state as a world-leading innovation hub for radiopharmaceuticals, radiodiagnostics, and theranostics to save the lives of Tennesseans and others far beyond,” said Rachel Patton McCord, an associate professor in the Department of Biochemistry and Cellular and Molecular Biology at UT.
The team will be building its capabilities with funding from the UT–Oak Ridge Innovation Institute, which was established in 2021 to enhance the long partnership between UT and ORNL.

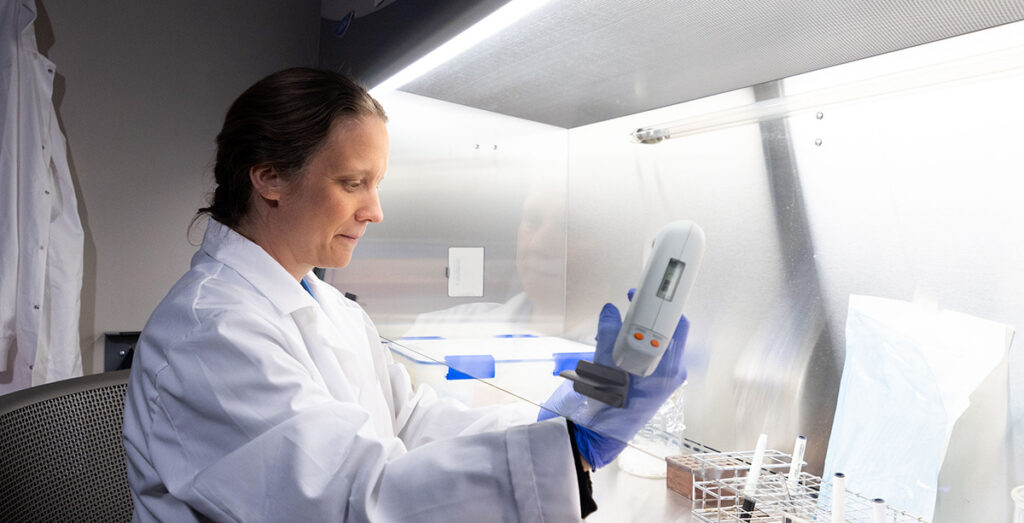
Sandra Davern
“UT–ORII provides us with the resources to recruit scientists across our institutions and will ensure that by working together on shared goals, we will maximize our impact,” said Sandra Davern, head of the ORNL Radioisotope Research and Development Section.
“Through this collaboration,” said Gabor Tigyi, Harriet Van Vleet Endowment Professor in Basic Oncology Research at the UT Health Science Center, “we are building a complete pipeline stretching across the entire state of Tennessee to research, generate, test, and apply novel targeted radioisotope treatments.”
In theranostics, radioisotopes are attached to molecules that are attracted to and accumulate around cancer cells. Imaging technologies track the location of the radioisotopes—and thus cancer—throughout the body. At the same time, the radioisotopes treat the cancer by releasing radiation where the cancer cells are located.
“This precision approach minimizes interaction with normal noncancerous cells,” Davern explained. “In contrast, chemo and other forms of radiation therapy cause both healthy and cancerous cells to experience stress, damage, or death.”

Gabor Tigyi
“Our focus is on radioisotopes that are very powerful, but only over very short distances and for short periods of time,” Tigyi added. “These are key properties for minimizing side effects.”
McCord, who studies DNA damage in human cells, pointed out the need to better understand the scientific basis of how radioactivity affects cells. “We want to be able to answer questions like when do cancer cells die, recover, or become resistant? How far will radiation travel and affect healthy cells in different situations? Answering these fundamental questions will help us to develop and produce new types of radioisotopes and explore their practical applications.”
“Bringing experts together from different disciplines is essential,” McCord added. “To succeed, we need radiochemists, cancer biologists, and experts in computation, imaging, and other fields.”
The radiophamaceutical team will receive $20 million in funding over five years to recruit and hire 20 experts. New hires will work in UT Knoxville’s College of Arts and Sciences, Tickle College of Engineering, and College of Veterinary Medicine, and in the UT Health Science Center.
“We will find people who complement and supplement our existing skill sets,” McCord said.
At UT Health Science Center, one of the first new hires will be an expert in cancer stem-like cells, a prime target for radioisotope treatment since they cause cancer to spread through the body and develop resistance to traditional radiation and chemotherapy.
UTHSC also plans to hire an expert in ovarian cancer biology to work alongside Junming Yue, an associate professor in the Department of Pathology. They will use animal models to test next-generation radioisotopes with a focus on treating ovarian cancer.
Another new hire will specialize in bioinformatics, using computational models powered by machine learning to analyze health data collected from cancer patients. Ultimately, bioinformatic analysis could help identify early markers of silent killers like ovarian cancer and identify better ways to target aggressive cancers with radioisotopes.
“However, there is a shortage of key expertise across the nation,” Davern said. “So we’re also thinking about how to bring in students, mentor them, and build the workforce we need.”
The team will tap existing UT degree programs, including the Bredesen Center’s Genome Science and Technology PhD program, to educate more students in these areas. “Our students will be marketable to academia, industry, and medical institutions. Building a notable center of strength here can attract more companies to Tennessee, too, giving UT graduates more in-state job options,” McCord said. “We want people to know Tennessee is where this work is happening and where we’re making real strides.”
“We’re at the beginning of something that can truly transform cancer treatment, especially for hard-to-treat cancers,” said Davern. “Together, UT and ORNL are creating solutions that benefit society—starting here in Tennessee.”